Losing sensation in your feet creates a silent threat that many people don’t pay attention to until it’s too late. Charcot foot develops when this loss of feeling allows ongoing damage, since you cannot sense discomfort or pain. However, medical professionals can identify this condition at different stages using specific diagnostic methods and visual cues. This article will walk you through how Charcot foot is diagnosed, the stages of Charcot, key early symptoms to recognize, and treatment options that can stop the condition from progressing.
What is Charcot Foot?
Charcot foot is a severe condition where nerve damage makes the bones of the foot weak and vulnerable to fractures. It occurs most commonly in people with diabetic neuropathy, who lose sensation in their feet. Healthcare providers often miss early diagnoses because patients do not feel any pain related to bone fractures, so the condition is mistaken for minor injuries like a sprain. The absence of pain allows people to go back to their normal activities and place weight on already fractured bones, which worsens the structural damage.
If left without proper treatment, Charcot foot progresses to serious foot deformities, ulcers that do not heal, dangerous infections, and eventual amputation. These problems develop because the damaged bone structure can no longer maintain the foot’s normal shape and function.
Causes and Risk Factors of Charcot Foot
Several medical conditions and lifestyle factors increase the chances of developing Charcot foot, a serious complication that destroys bones and joints. Here are some of the main causes and risk factors:
Diabetic Peripheral Neuropathy
High blood glucose levels damage nerve fibers over time, especially in the feet and legs. This nerve damage makes people insensitive to feeling sensations like pain, heat, cold, or pressure in their extremities. As a result, when neuropathy develops, people cannot sense when their foot is cut, bruised, or fractured during daily activities. Without pain as a warning signal, injuries continue to worsen as people continue walking on damaged bones and joints.
Repeated Microtrauma to the Foot
Walking on rough surfaces, wearing tight shoes, or stepping on small objects creates tiny stresses on foot bones and joints. In healthy people, these minor stresses cause discomfort that leads to automatic adjustments in their walking or standing position. Without protective nerve function, these small daily stresses add up to stress fractures and joint dislocations over weeks and months. The altered mechanics of the feet of people with diabetic neuropathy distribute weight abnormally, leading to pressure points that can cause bone breakdown in specific areas.
Poor Circulation
Diabetes damages blood vessels throughout the body through a condition called autonomic neuropathy, which disrupts the normal control of blood flow. As circulation to the feet is reduced, injured tissues cannot receive sufficient oxygen and nutrients required for healing. This dysfunctional healing process allows small injuries to persist and become serious complications. Poor circulation also weakens bone structure and makes fractures more likely.
Obesity
Carrying excess weight dramatically increases the force placed on the bones in the foot during movement. Research shows that each additional pound of body weight creates approximately eight pounds of extra pressure on the feet and ankles during walking. This multiplied force effect becomes especially destructive when it combines with the inability to sense when bones and joints exceed their stress capacity.
Long-Standing Diabetes
The duration of diabetes directly correlates with the deterioration of nerves and blood vessels throughout the body. People who have managed diabetes for more than seven years show progressively worse complications because prolonged high blood sugar causes cumulative damage over time. Additional risk factors like tobacco use and alcohol consumption accelerate this damage. Research indicates that about 1% of people with diabetic nerve damage will develop Charcot foot.
3 Stages of Charcot Foot
The three main stages of Charcot foot are as follows:
Stage 1: Fragmentation/Development (Acute Phase)
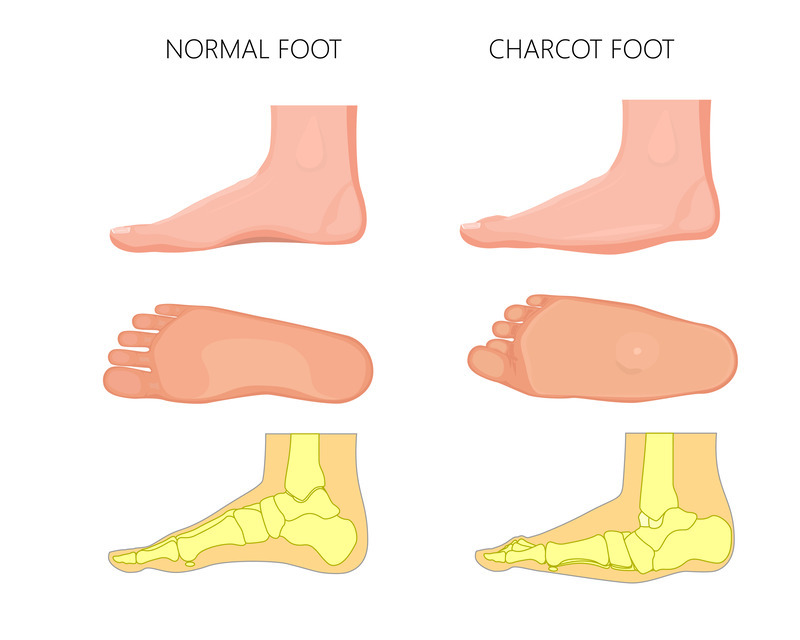
During the initial stage, the foot becomes noticeably red, swollen, and warm compared to a healthy foot. Small bone fractures start occurring internally while soft tissues swell around the joints. The bones lose their strength and may become soft, causing joints to move out of place. The bottom of the foot can appear flat or curve abnormally, with hard bumps sticking out.
Stage 2: Coalescence (Subacute Phase)
The redness, swelling, and warmth gradually go away as the body tries to fix the damage in the second stage. Broken bone pieces start fusing back together while the destruction process slows down.
Stage 3: Consolidation (Chronic Phase)
Finally, in the last stage, inflammation completely disappears as the bones solidify into their new positions. Unfortunately, the foot doesn’t return to its original position and remains twisted. The changed shape makes it easy for sores to form on the bottom of the foot. These sores can become serious problems that might need surgery if they are not treated properly.
Early Symptoms to Watch For
As Charcot foot can easily go unnoticed or be dismissed as a minor issue, recognizing these early visual and physical signs becomes critically important. The following symptoms require a visit to your doctor:
Sudden Swelling in One Foot or Ankle
One of the most common first signs of Charcot is when your foot begins swelling without any clear reason or injury. This happens as the internal structure of your foot starts to weaken, causing inflammation that you can see but may not feel. You might initially experience this problem when trying to put on regular shoes and finding that they no longer fit comfortably.
Warm to the Touch
When you place your hands on both feet, the sore foot will be noticeably warmer than your other foot. This temperature difference is because your body is channeling more blood to repair damage happening inside your foot.
Redness Without Pain
The skin on your affected foot may become red or discolored, and you might observe that it’s a different color from your other foot. This redness appears as your body responds to bone and joint problems developing inside. However, you won’t feel the pain that would normally accompany such changes. Many people can find this lack of pain baffling, but it’s actually typical when you have nerve damage.
Collapsing Arches
If Charcot foot goes untreated, the natural arch in your foot can eventually collapse and become completely flat. This progression creates what is known as a rocker-bottom foot, where the middle of your foot may actually bulge downward instead of curving upward like a normal arch.
Diagnosing Charcot Foot
Charcot foot diagnosis is challenging since the initial symptoms often resemble common injuries or infections. When specialists recognize Charcot in the early stages, they can start preventive treatment to avoid severe complications before patients develop extreme foot deformities that may lead to amputation. These are the main ways through which doctors diagnose this condition:
Physical Exam and Clinical History
Your doctor will start by asking specific questions about your Charcot symptoms and how they developed. They will ask about your diabetes history, including how well your blood sugar has been controlled, and whether you have had previous foot problems. The physical exam focuses on finding three significant warning signs: unusual warmth, redness, and swelling in your foot.
Imaging Tests
Doctors use different types of scans to see what’s happening to your bones and tissues. These tests help confirm a diagnosis and rule out other conditions that might cause similar symptoms.
X-Rays
X-ray images show your foot’s bone structure and can detect fractures or displaced bones. However, these photos can appear completely normal during the early stages of Charcot foot. As the condition progresses, X-rays become more helpful by showing broken bones, joint damage, and foot deformities.
MRI
MRI scans help doctors to see inside your foot without surgery, clearly showing both bones and soft tissues. This is a very useful test because infections can look just like Charcot foot in the early stages. When doctors have a clear view of your foot’s internal structures, they can more easily distinguish between these two conditions.
Bone Scans
CT scans produce high-definition, three-dimensional images of your bones, which help foot surgeons plan surgery if it is needed. Bone scans use a small amount of radioactive material to detect areas of your bones that are more active than normal, which may indicate infection or inflammation. Doctors typically order these advanced tests when simpler imaging doesn’t provide clear results or when they need very detailed information about your foot’s health.
Treatment Options for Charcot Foot
Treating Charcot foot aims to create stability in the foot to prevent further damage or injury. The goal is to help patients use regular diabetic shoes for daily activities. Here are the main treatment options available:
Non-Surgical Treatments
Non-surgical treatment starts with protecting the foot using special casts or boots to prevent further damage. Total contact casts cover the whole foot and work better than regular casts because they reduce swelling and prevent bones from shifting into worse positions. Patients must stay completely off their feet during this time. This means using crutches, wheelchairs, or knee walkers for daily activities.
The healing process takes about three months or longer, and doctors might change the cast every week or two as the swelling goes down. After bones start healing properly, patients can switch to heavy-duty removable boots. These boots still protect the foot but allow for cleaning and examination.
Custom orthotics and special braces become important after healing because they support a healthy foot shape and prevent new deformities from forming. Additionally, keeping blood sugar levels under strict control helps the bones heal quickly and reduces the risk of infections or other serious complications during treatment.
Surgical Treatments
Surgery becomes necessary when the foot becomes unstable or when severe shape changes make walking impossible without developing ulcers. Reconstructive foot surgery corrects major deformities by using plates, screws, and rods to hold bones in better positions while they heal.
Bone fusion operations permanently join damaged bones together. This creates stability in areas where bones have shifted out of place. Realignment procedures involve cutting bones and moving them back to normal positions. These procedures often require more metal hardware than regular foot surgery because diabetes weakens bones.
These operations carry higher risks of wound problems and infections compared to normal foot surgery. Patients must avoid walking until doctors say it’s safe. In severe cases with deep bone infections, loss of blood supply, or ulcers that won’t heal, amputation may be the only way to save the patient’s life and help them maintain mobility with a prosthetic device.
Living With Charcot Foot
In addition to surgical and non-surgical treatments, living with Charcot foot means adapting your daily activities and foot care routine. These changes help reduce stress on your feet while keeping you safe and active at home. Here’s how to cope with this condition effectively:
Lifestyle Adjustments to Reduce Stress on Your Foot
When you maintain a healthy weight, it takes the pressure off of your feet and gives damaged bones a better chance to heal properly. Good nutrition with calcium and vitamin D rebuilds bone strength. Stopping smoking improves blood circulation to your feet. Control alcohol intake and maintain healthy blood pressure to support your body’s natural healing process.
Regular Foot Checks and Diabetic Foot Care
Daily foot checks help you catch problems early when they’re easier to treat. Examine every part of both feet carefully, including the spaces between your toes. Use good lighting or a mirror to see areas that are hard to reach. Proper nail care prevents painful ingrown toenails that could become infected.
Importance of Patient Education and Compliance
Understanding your condition gives you the power to make wiser decisions about protecting your feet throughout the day. Follow your doctor’s advice and use mobility aids like crutches or wheelchairs to prevent further bone damage.
Long-Term Use of Protective Footwear
Prescription footwear designed for your specific foot shape protects against dangerous pressure points and ulcers. Wear these protective shoes consistently throughout the day, along with properly fitted socks, to help prevent injury. Custom-made shoes become necessary when foot deformity is severe, ensuring proper support and comfort for your changed foot structure.
Preventing Charcot Foot in Diabetics
Your risk of getting Charcot foot increases when you’ve had diabetes for a long time or already have nerve problems in your feet. The encouraging news is that you can take steps to lower this risk and protect yourself from this condition:
Early Screening for Peripheral Neuropathy
Testing for nerve damage early on helps your doctor identify issues before they become bigger problems. Talk with your doctor about scheduling these tests to ensure you get the right care at the right time.
Monitoring Foot Temperature and Appearance Daily
Examine your feet each day for changes like heat, swelling, or unusual coloring that damaged nerves might prevent you from feeling. Special temperature tools can show you early signs of trouble that aren’t yet visible to your eyes.
Regular Podiatric Visits
Professional podiatric check-ups help catch problems that you might miss during home examinations. Having these appointments once a year benefits most people with diabetes, while those with additional risk factors should consider visiting more often.
Final Thoughts
Charcot foot develops through three specific stages, where nerve damage prevents patients from feeling bone fractures and joint destruction in their feet. Without proper medical care, this condition can lead to permanent deformity and serious complications that can threaten your mobility and independence. Dr. Gary Driver offers expert Charcot reconstructive surgery, which reduces foot pain, increases stability, corrects deformities, and helps patients return to normal life. If you suspect you have Charcot foot symptoms, schedule an appointment today!
Frequently Asked Questions (FAQs)
What are the early signs of Charcot foot?
The most common first signs include one foot becoming noticeably warmer than the other, along with redness and puffiness. Getting medical help quickly when you spot these changes can prevent the condition from getting much worse.
How can I tell the difference between Charcot foot and an infection?
Charcot foot typically occurs without any open wounds on your skin, while infections usually involve cuts or broken skin areas.
Why does Charcot foot occur?
When diabetes or other diseases damage the nerves in your feet, you lose your body’s natural alarm system for injuries. Small problems that would normally hurt enough to make you rest instead go unnoticed and get worse each day. Eventually, this constant stress causes your foot bones to crack and shift out of their normal positions.
What happens if Charcot foot is left untreated?
Your foot bones will keep fracturing and shifting into abnormal positions that make normal walking impossible. This bone collapse often creates pressure points that turn into open sores, which can then become seriously infected.
Can I walk with Charcot foot?
No, walking will likely cause more fractures and make your condition significantly worse. You’ll need to use wheelchairs, walkers, scooters, or crutches to get around while your foot heals.
How long does Charcot foot take to heal?
Most people need between six months and a full year for complete recovery. The timeline depends on how well you avoid putting weight on your foot and how damaged it was when treatment started.
How can I prevent Charcot foot if I have diabetes?
Keeping your blood sugar under control helps slow down nerve damage that can lead to Charcot foot. Daily foot checks and wearing shoes that fit well are equally important for catching issues before they become serious.